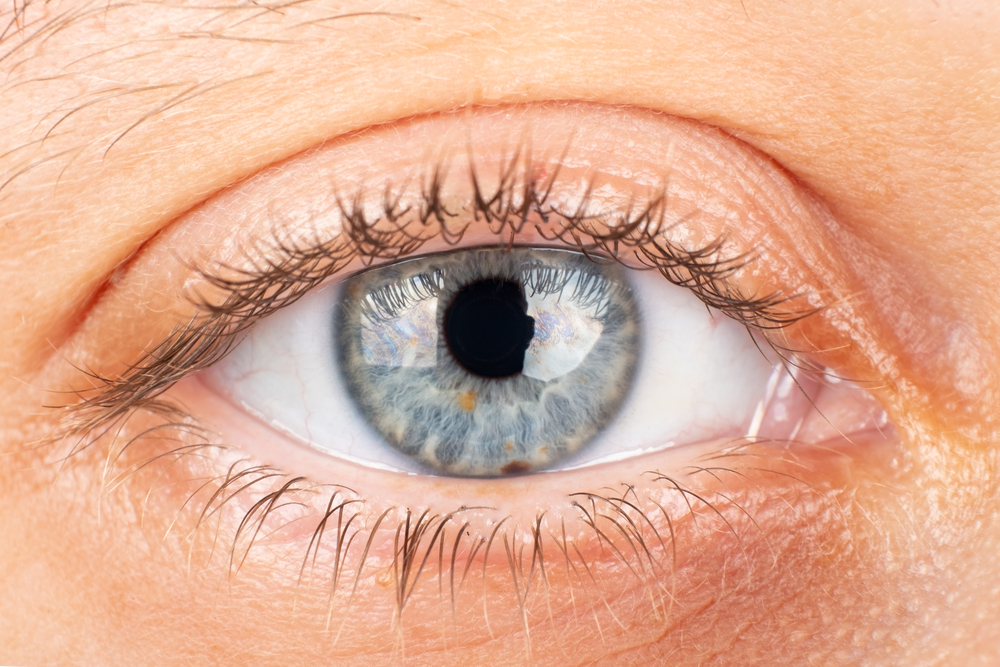
Keratoconus is a progressive eye disease in which the cornea — the clear front part of the eye — gradually thins and begins to bulge into a cone-like shape. This irregular shape prevents light from focusing properly on the retina, leading to distorted and blurry vision. It can affect one or both eyes and often progresses asymmetrically.
Although once considered rare, studies now show that keratoconus is more common than previously believed. It typically appears in adolescence or early adulthood and may worsen over time at varying rates.
Common Symptoms of Keratoconus
The symptoms of keratoconus vary by stage. Early on, patients may notice:
- Frequent changes in eyeglass prescriptions
- Blurred or cloudy vision
- Glare and light sensitivity
- Headaches or eye strain
As the condition progresses, patients may develop corneal scarring, increased myopia, and irregular astigmatism that glasses can’t correct.
For more on symptom patterns and what to look for, see our article on keratoconus symptoms and diagnosis.
How Is Keratoconus Diagnosed?
An accurate diagnosis typically requires a comprehensive eye exam, including tests like corneal topography and tomography. These advanced scans provide detailed maps of the cornea’s curvature and thickness.
In early stages, an optometrist may detect subtle signs such as an irregular astigmatism or asymmetric distortion in vision. In later stages, classic indicators like the Fleischer ring (iron-colored ring at the base of the cone) or Vogt’s striae (stress lines in the cornea) may appear.
Curious about how mapping technology supports diagnosis? Learn more in our article on corneal mapping for keratoconus.
What Causes Keratoconus?
While the exact cause is unknown, both genetic and environmental factors seem to play a role. About 1 in 10 people with keratoconus have a first-degree relative with the condition, although it’s not strictly hereditary.
Keratoconus is more common in people with allergies, asthma, eczema, or those who frequently rub their eyes.
How Does Keratoconus Affect Vision?
In early stages, vision may still be functional with glasses or soft contact lenses. But as the cornea becomes thinner and more irregular, vision deteriorates. In advanced cases, patients may require specialty treatments like scleral lenses, which create a smooth optical surface over the cornea and restore clear vision.
These lenses are ideal for irregular corneas and severe cases—read more on our dedicated page for scleral lenses.
Advanced Treatment Options
Today’s treatment plans are highly individualized. In early stages, prescription glasses or RGP lenses may suffice. As the disease progresses, options expand to:
- Corneal Cross-Linking (CXL): Slows or halts disease progression
- Scleral lenses: Custom-designed for severe distortion
- Corneal transplants: Reserved for advanced scarring
Looking for a fully customized solution? Explore our innovation with EyePrintPRO – ideal for highly irregular corneas and sensitive eyes.
Expert Care Matters
Early and accurate diagnosis is key. If you suspect keratoconus, schedule an assessment with a trusted keratoconus specialist at M’Eye Clinic. Our approach combines cutting-edge technology, in-depth expertise, and a personalized treatment plan designed to preserve your vision.
MyClinic is a trusted center for advanced eye care in Jerusalem, providing expert keratoconus diagnosis and treatment to patients from across the Middle East — including the UAE, Saudi Arabia, Qatar, Bahrain, Kuwait, and Turkey.