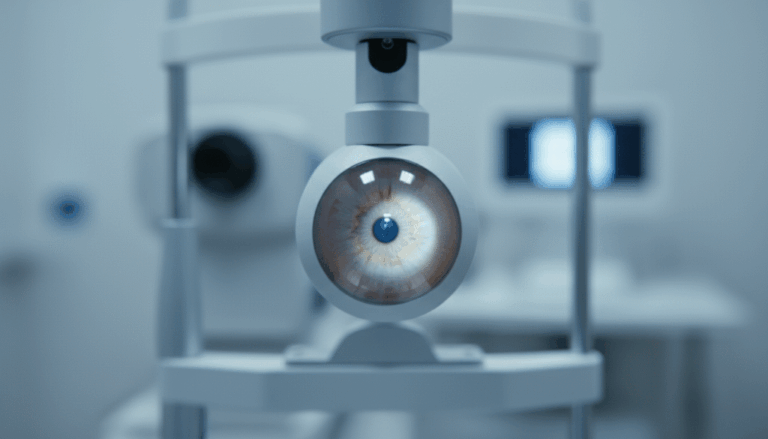
Keratoconus is a progressive condition in which the clear corneal tissue thins and bulges forward, becoming cone‑shaped instead of round. In the early stages, vision can often be corrected with glasses or soft contact lenses. In its advanced stages, however, the cornea becomes so irregular that ordinary solutions no longer work. In Israel and across the Middle East, many patients with advanced keratoconus feel lost, as if nothing can be done and surgery is the only option. This article explains why that is not true.
What happens in advanced keratoconus?
In advanced keratoconus the cornea is unstable, thin and irregular. Patients experience rapidly deteriorating vision, extreme light sensitivity, double vision and distortions that make reading and driving difficult. At this stage, the corneal surface develops both geometric irregularities and high‑order aberrations (HOA—optical distortions that cannot be corrected with spectacles or ordinary lenses).
Not long ago, many patients were sent straight to corneal transplant. Today, advances in imaging and customised scleral lens technology have opened new possibilities. At M’Eye Clinic we use ultra‑wide corneal tomography, high‑resolution anterior OCT and dynamic aberrometry to measure the cornea and the optical wavefront. This allows us to design lenses that neutralise not only the regular astigmatism but also complex HOA, giving patients sharp, stable vision again.
Treatments for advanced keratoconus
- Custom scleral lenses and EyePrintPRO®: These large lenses vault over the entire cornea and rest on the white of the eye (sclera). By creating a fluid reservoir over the irregular cornea, they smooth the optical surface and correct aberrations. In cases of extreme irregularity we may take a 3D impression of the ocular surface (EyePrintPRO) to design a fully bespoke lens.
- Wavefront‑guided lenses: When standard scleral lenses aren’t enough, we use aberrometry to measure the high‑order aberrations and create a lens with a front surface that neutralises them. This can dramatically improve night vision, reduce halos and restore clarity.
- CXL (corneal collagen cross‑linking): In progressive keratoconus, stiffening the cornea with UVA light and riboflavin can halt the disease.
- Corneal transplant or deep lamellar keratoplasty: For very thin or scarred corneas, surgery may eventually be required. Even then, customised scleral lenses are often used after the transplant to fine‑tune vision.
Living with keratoconus: our approach
At M’Eye Clinic we believe no one should be told that nothing more can be done. Every patient undergoes a full evaluation of corneal shape, biomechanics and optical quality. We then discuss the therapeutic options and build a custom rehabilitation plan.
If you suffer from irregular vision, glare or difficulty driving at night despite wearing the “correct number”, you may have advanced keratoconus or another corneal disorder. There are treatments beyond glasses and standard lenses. Contact us for a comprehensive assessment and discover what is possible.