Keratoconus is a progressive eye disease in which the tissue of the cornea gradually weakens and thins, causing it to bulge outward into a cone-like shape. This condition affects approximately 1 in 2,000 people and typically begins during the teenage years or early adulthood, with gradual progression over time.
The causes of keratoconus vary. For some, it runs in the family. For others, it can be triggered by frequent and aggressive eye rubbing, chronic allergies, or underlying medical conditions. In rare cases, it may appear after laser eye surgery performed without adequate screening.
Symptoms of Keratoconus
Keratoconus usually causes vision to deteriorate slowly and asymmetrically (with one eye being worse than the other). While it doesn’t typically lead to complete blindness, it can cause significant dependence on glasses or scleral contact lenses.
Early signs include:
- Gradual vision decline in one or both eyes
- Double vision when looking through one eye
- Blurry or distorted vision at all distances—even with glasses or contacts
- Halos and glare around lights, especially at night
How Is Keratoconus Diagnosed?
If you’re experiencing any of the symptoms above, it’s important to see an optometrist who specializes in corneal conditions. A thorough eye exam can determine whether you have keratoconus or a similar disorder.
The diagnosis usually involves corneal mapping (topography or tomography), which generates a 3D image of the cornea’s shape and thickness. This process is quick, painless, and non-contact.
Early detection is key to monitoring the condition. If keratoconus progression is found, treatment can help prevent further damage. Patients considering laser eye surgery must be screened for keratoconus risk to avoid complications.
What Are the Treatment Options?
Treatment depends on the stage of the disease. In early stages, glasses with astigmatism correction may be enough. But as keratoconus progresses, vision can often only be corrected using rigid gas permeable or scleral lenses.
If thinning continues, the main goal becomes stabilizing the cornea. The most effective method today is corneal cross-linking, which strengthens the cornea and halts progression.
What Is Corneal Cross-Linking?
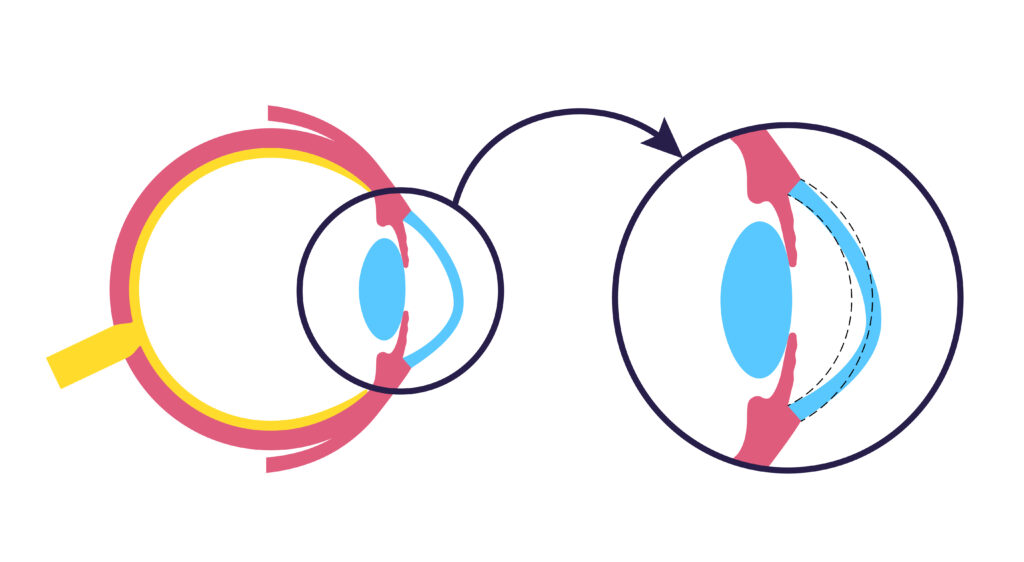
In healthy corneas, natural collagen fibers are cross-linked to maintain structural integrity. In keratoconus, these cross-links are weakened or missing, allowing the cornea to bulge.
Cross-linking treatment reinforces these connections by adding new “cross beams” that strengthen the cornea, helping it retain shape and focus light more accurately.
Other Treatment Options
In certain cases, a plastic ring implant (Intacs) may be inserted into the mid-layer of the cornea to reshape it and improve vision—especially in patients who struggle with lenses.
The most advanced solution today is custom scleral lenses. These are specially designed to fit the unique contours of keratoconic eyes, offering hydration, comfort, and excellent visual correction. They are available in multiple designs including mini scleral lenses.
For recommendations, consult a keratoconus specialist who can match you with the ideal solution.
Can Keratoconus Cause Blindness?
If left untreated, keratoconus can progress to the point where irreversible damage occurs. Although most patients do not go fully blind, vision can become severely impaired. At advanced stages, scarring may develop on the cornea, which cannot be corrected by glasses, and in some cases even cross-linking is no longer effective.
In these situations, either hard contact lenses or corneal transplant surgery may be necessary.
Final Thoughts
Early diagnosis and proper treatment are essential. When caught in time, keratoconus can be managed successfully—often avoiding surgery and maintaining excellent quality of life.
Don’t wait until symptoms worsen. Book an appointment with a keratoconus specialist at M’Eye Clinic. With advanced diagnostics, personalized treatments, and innovative technology, we help patients across the region protect their vision—before it’s too late.